University of Idaho research may slow antibiotic resistance to drugs
New research from the University of Idaho has identified two genetic mutations in bacteria that help explain how some bacteria evolve and retain resistance to multiple antibiotics.
The results, published Aug. 7 in Nature, could play a role in helping scientists slow or stop the spread of antibiotic resistance to multiple drugs, something responsible for 2 million infections and 23,000 deaths in the U.S. every year, according to the Centers for Disease Control and Prevention.
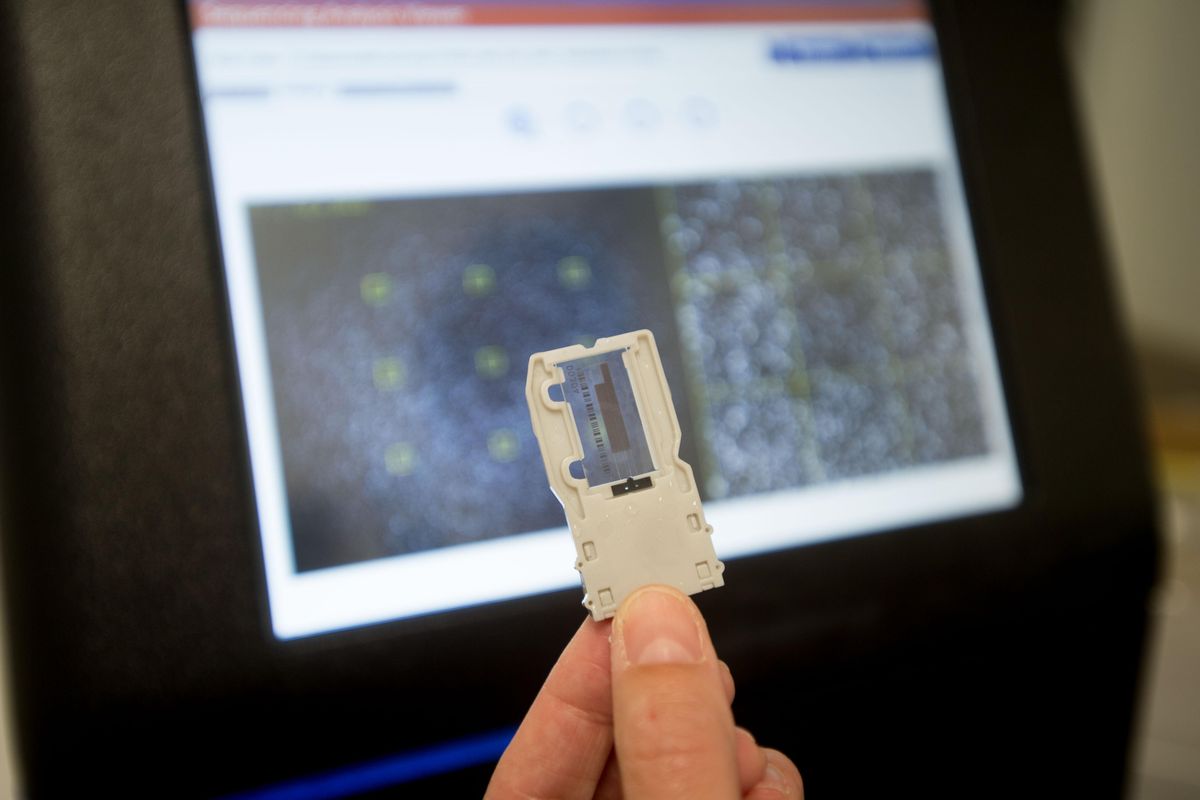
The team, led by Eva Top, a professor at the university’s Department of Biological Sciences, focused on plasmids: small pieces of DNA that can be transferred between bacteria cells.
Plasmids aren’t part of a bacteria’s chromosomes and geneticists who study bacteria can tell plasmids apart from a bacteria’s own chromosomes. But they allow bacteria to transfer traits, including antibiotic resistance, from one bacterium to another.
“A bacterium that is sensitive to a set of antibiotics can within a few minutes time become resistant … because it receives this plasmid from other bacteria,” Top said.
Plasmids aren’t the only way for bacteria to become resistant. Bacteria can also evolve through mutations in their own chromosomes, which may give some bacteria resistance to a particular drug, allowing those bacteria to survive and reproduce if the whole population is exposed to the antibiotic.
But plasmids are unique because they can give a bacterium resistance to multiple drugs at once, even if the bacterium has never encountered those drugs.
“They’re picking up a lot of antibiotic resistance genes and spreading them because of our habits of using so many antibiotics,” Top said.
If plasmids were that simple, you’d expect most bacteria to be resistant to most antibiotics. But acquiring plasmids also carries a cost. Lugging around extra DNA can slow reproduction and growth because bacteria have to make more proteins to express that DNA. So if bacteria have plasmids they’re not using, they might shed them.
Top’s team wanted to see what makes some bacteria hang on to plasmids, and therefore to antibiotic resistance, more easily than others. They found two genetic mutations can help bacteria lower or even eliminate the cost of keeping plasmids, turning a net cost into a net benefit.
“It suggests that this may be a rather common way for bacteria to adapt to these multidrug-resistant plasmids,” Top said.
Once bacteria had evolved to hang on to plasmids, the team tried taking those plasmids away and replacing them with other plasmids that conferred resistance to different drugs. They found the bacteria held on to those new plasmids better as well.
Having a better idea of the way bacteria evolve with plasmids could help scientists target multidrug resistance more effectively. The fact that the same mutations lead bacteria to hold on to multiple types of plasmids makes it easier to develop a single drug to target that mutation.
One possibility might be developing a drug to make bacteria shed the plasmids they’ve acquired, then hitting them again with an antibiotic they’re now vulnerable to, Top said.