Kreidler sets new signup period because of health exchange problems
A special enrollment period will last from Wednesday through Nov. 14, allowing customers with unresolved problems to sign up for different plans or with different companies. There’s a catch: They could lose their subsidies or any deductible credits or out-of-pocket expenses they've built up with their current plans. But for people unable to straighten out problems with payments, claims or billings for their current plan, re-enrollment in a different plan would give them coverage, Insurance Commissioner Mike Kreidler said.
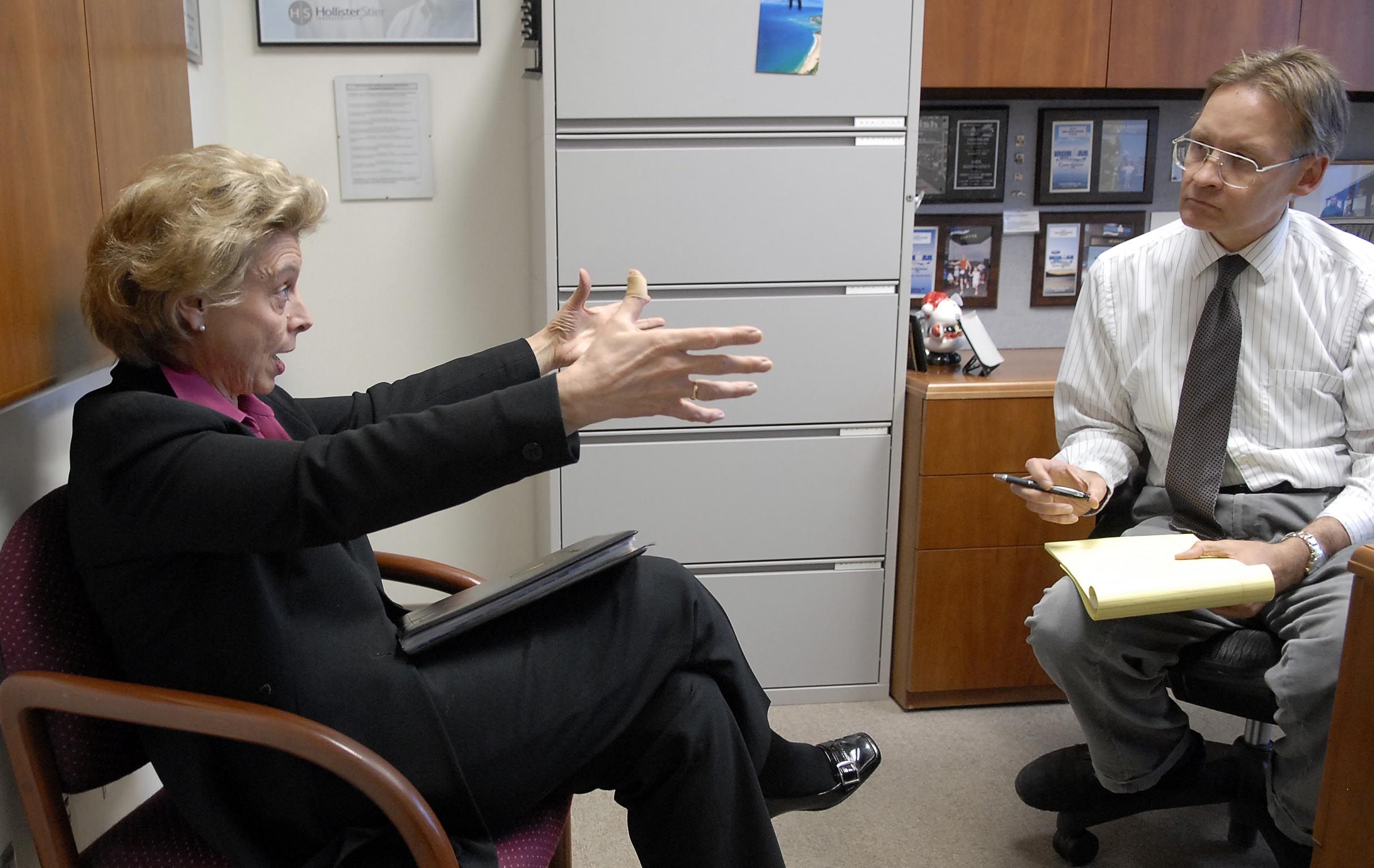
“It's not a perfect solution,” Kreidler said. “But it’s an option.”
Health exchange officials argued it wasn't a good option for most people...
To read the rest of this item, or to comment, continue inside the blog.
The Washington Healthplanfinder – which helps link residents who don’t have health insurance through a job or another government program to plans offered by different companies – announced last month it had problems with an estimated 6,000 accounts. Some customers had paid their premiums to the exchange, but were getting notices from their carrier that they were being cancelled for non-payment. Others were told they needed to supply information that they had already submitted. Exchange officials said the problems were a combination of software issues and human error and vowed to make major changes by the end of August.
Earlier this month, they said customers with billing problems could make payments directly to the insurance carrier.
On Monday, Exchange Chief Executive Officer Richard Onizuka and Exchange Board Chairman Ron Simms issued a joint statement that an “aggressive action plan” had resolved problems with 6,000 accounts of customers who had problems using their coverage and 12,000 customers who still had coverage but experienced billing or payment problems. More fixes to the system will be made by late this week with more expected in September.
But Kreidler said his office continues to get complaints from customers even though his agency has no control over the exchange. “I’m not overly confident they’re going to resolve this in the next couple of months,” he said.
He does have the authority to declare special enrollment periods that allow customers who meet certain conditions to sign up for new insurance policies outside the open enrollment period. The most recent open enrollment ended March 31 and the next one doesn’t start until Nov. 15.
Some situations allow families to sign up through the exchange at any time, such as loss of job, marriage, divorce, birth in the family or moving to Washington. Starting Wednesday, customers who can show they have billing or payment problems will be able to take part in a special enrollment period with several options.
They can “reset” their plan inside the exchange, essentially cancelling the current plan and signing up a new one with the same insurance company. In doing this, they might lose any credits toward their deductible or out-of-pocket payment requirements.
They can switch to a different insurance company’s plan within the exchange. In doing this, they could lose their credits and the subsidy amount might change.
They can go to their insurance company or a different company and switch to a plan sold outside the Exchange. In doing this, they would lose any subsidy they are currently receiving and lose any credits. Claims on their old policy might not be covered if they terminate coverage with the exchange, the prepared statement form Onizuka and Simms warned.
The special enrollment period may only help a small number of customers who are having problems, the prepared statement said.
People who are not receiving a subsidy or haven’t come close to meeting their copayment threshold might be willing to work through an insurance company, while those who get a significant a subsidy or have met their threshold might not want to start all over, Kreidler said. But even if the special enrollment period only helps a few people, it’s worth setting it up, he added.