More people covered, costs lower for Washington Health Plan
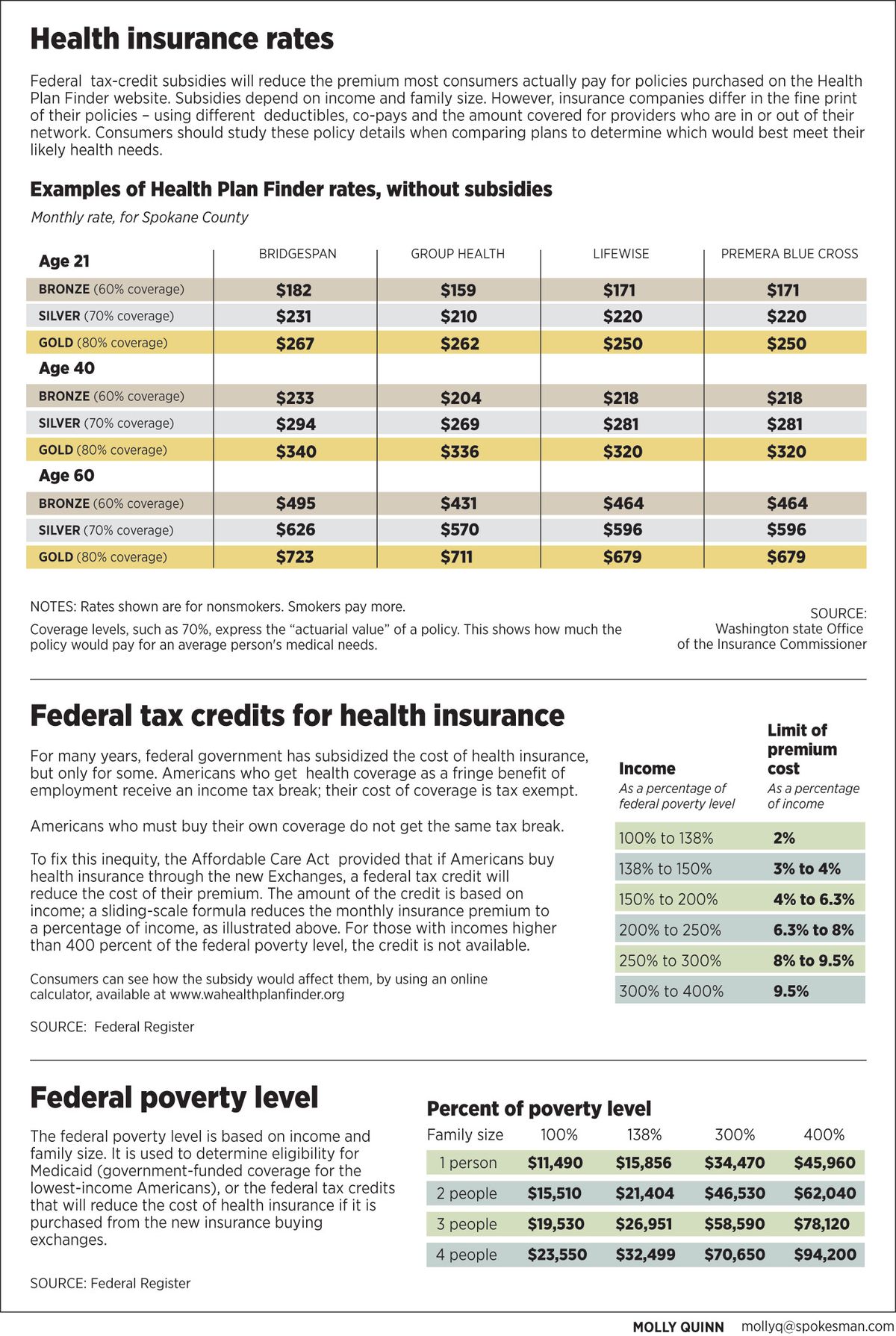
Going shopping: Washington health plan shoppers can expect to receive 80 percent coverage of their average medical needs if they purchase a gold plan, 70 percent coverage with the purchase of a silver plan and 60 percent coverage with a bronze plan.
What will Obamacare cost, and who will it help? In Washington state, where final rates emerged this week, it will cost less, cover more people, and provide more comprehensive benefits than consumers get today.
On Thursday, the office of state Insurance Commissioner Mike Kreidler announced its final decisions on the rates and policies to be offered for sale on Washington’s new insurance-selling website, the Health Plan Finder.
Located at http://www.wahealthplanfinder.org, the site is already running. The new rates are not on it yet, however, and insurance sales will not begin until Oct. 1. The policies it sells will take effect starting Jan. 1.
Only four of the nine insurance companies who sought regulatory approval passed muster. All four whose plans won approval will operate in the biggest counties, including Spokane. Residents of smaller counties will have fewer choices.
Still, Kreidler said he was pleased. With this being the first year, and with federal agencies issuing rule clarifications as recently as a few weeks ago, it has been difficult for regulators and insurance companies to figure out what federal law requires, he said.
It is clear, Kreidler said, that more insurance companies want to be in the game and will file proposals for 2015.
In addition to selling health insurance to paying customers, the Health Plan Finder site will become the way Washington residents sign up for Medicaid, the government-funded health plan for low-income people. The Washington Legislature decided to expand Medicaid for 2014, making it a comprehensive plan covering everyone up to 138 percent of federal poverty level. The federal government will pay most of the cost.

Thursday’s announcement affects uninsured people with incomes too high to qualify for Medicaid.
In Washington, that’s more than 507,000 people, not including the 328,000 uninsured people who will be eligible for expanded Medicaid, according to state and federal estimates.
The final insurance rates mark a big milestone on the road to the Affordable Care Act’s vision of expanded health care coverage.
Today, people without insurance can get some types of care in hospital emergency rooms, where costs are high and get passed along, via hospital fees and insurance rates, to those who do have coverage. But when the uninsured experience serious medical problems, the bills often push them into bankruptcy; medical costs account for 60 percent of personal bankruptcies in the United States. And, due to the inability to pay for care, many ailing Americans simply go without it and die: According to the American Journal of Public Health, lack of insurance is linked to 44,789 deaths per year in the United States.
It was to address those problems that the Affordable Care Act of 2010 required Americans to get health insurance and provided for the creation of government-run websites to sell it. Private-sector health insurance companies provide the coverage these websites sell. For most consumers, federal subsidies will reduce the cost of coverage.
Over the past several months, Kreidler’s actuaries have gone back and forth with the insurance companies, he said, scrutinizing the proposed rates. The office makes sure the rates are appropriate – high enough to cover the promised benefits, and not so high as to overcharge consumers.
The final rates dropped about 2 percent as a result of these discussions – an amount that will save Washington consumers more than $10 million, Kreidler said.
Approved for sale on the Health Plan Finder were policies from Bridgespan, Group Health Cooperative, Lifewise and Premera Blue Cross. Bridgespan is owned by Regence Blue Shield. Lifewise is owned by Premera.
Rejected were policies from Moda Health Plan Inc., Kaiser Foundation Health Plan of the Northwest, Community Health Plan of Washington, Coordinated Care Co. and Molina Healthcare of Washington Inc.
“Several of them (insurance companies) struggled to guarantee access to certain providers and hospitals,” Kreidler said. “It’s our duty to make sure that if you buy a health plan, you can actually see the doctor or hospital that provides the service you need. This was a challenge for some of the insurers new to the commercial market.”
Due to federal regulations, the policies that won approval feature considerably more coverage than has been available in the past. In recent years as medical costs have soared, individual policies have covered less and less, Kreidler says, to a point where they cover perhaps 40 percent of medical bills and often do not cover maternity care or drugs at all.
This difference in benefits makes it difficult to compare today’s available policies to the ones on the exchange website.
For next year, consumers can choose whether they want coverage of 60 percent, 70 percent or 80 percent. For buyers under age 30, it will be possible to purchase a high-deductible policy. Only one carrier – Group Health – secured approval for a high-deductible plan.
Also, federal rules require all policies to cover 10 “essential benefits”: ambulatory services, emergency services, hospitalization, maternity and newborn care, mental health, prescription drugs, rehabilitation, laboratory services, prevention and wellness, and pediatric services including dental and vision care.
When an economist in Kreidler’s office compared the new plans to the individual policies available now, he concluded the new plans would cost less in most age brackets – taking into account the high deductibles in use today and the impact those deductibles have on a consumer’s out-of-pocket medical bills.
Some companies whose plans won approval do not sell policies in every area of the state.
• Only one, Lifewise, plans to sell coverage in all 39 counties of Washington.
• Premera Blue Cross plans to sell coverage in all counties except Clark County.
• Group Health Cooperative plans to sell coverage in 19 counties: Benton, Columbia, Franklin, Island, King, Kitsap, Kittitas, Lewis, Mason, Pierce, San Juan, Skagit, Snohomish, Spokane, Thurston, Walla Walla, Whatcom, Whitman, and Yakima.
• Bridgespan plans to sell only in seven counties: King, Kitsap, Pierce, Skagit, Snohomish, Thurston and Spokane.
More work remains before the public readily can see all of the insurance rates approved this week. The state Health Benefit Exchange, which operates the Health Plan Finder, must grant its own approval to the rates and expects to do so on Aug. 21. Next, programmers must load the rates into the website, together with complete details about each competing policy.
For the time being, one of the most complex calculations for consumers to make involves the federal tax credit, which will reduce the cost of premiums. The tax credits are calculated on a sliding scale, with the size of the credit affected by family income and the cost of the policy. Credits are available up to 400 percent of federal poverty level.
After the Health Plan Finder site has loaded all the information, consumers will be able to enter their income, pick a policy and see immediately whether they qualify for a subsidy and how much it would be.
Rough estimates of the tax subsidy are available now from a calculator on the Health Plan Finder website. But these estimates are based on rates higher than insurers actually proposed.
An updated example: For a family of two 40-year-olds and two children, with an income of $49,000 a year, one of the new Group Health policies would cost $858 per month; but this family could get a $593 subsidy, reducing its monthly premium to $265. Now that the rates are in hand, solid numbers are expected on the Health Plan Finder by Oct. 1.